Let’s talk about your contraception
Do you need contraception? Do you use contraception? What influences your choices when thinking about your options? There’s lots to consider.
Did you know that up to half of all Australian women will have an unintended pregnancy in their lifetime? In a recent study, 60% of Australian women who had an unintended pregnancy were using at least one form of contraception – 43% were on the pill at the time.
The invention of “the pill” was a game changer for family planning that became widely available in Australia in the 1960s. Since then, many generations of Australian women have been turning to the pill to prevent unintended pregnancies (contraception), or as part of treatment for acne, skin concerns, heavy menstrual bleeding, endometriosis and premenstrual syndromes. Lots of women choose the pill because their friends, sisters and mothers did – so it is more familiar.
However ladies – times have changed, and the pill is not the most effective contraception option anymore. It might still be the right choice for you – but other choices that are more effective include the implant, the intrauterine device, and the injection. Don’t want a long-acting method but hate taking the pill every single day? There is also a soft plastic ring that is inserted once a month into the vagina and remains there for 3 out of every 4 weeks – talk about a time saver. Condoms are the only way to protect against infections and are non-hormonal, but are only 88% effective (typical use).
So how do you know what is right for you?
- Make a list of what is important to you (effectiveness, possible side effects, previous experience, costs, convenience, etc)
- Check out the table below – comparing the two most effective options with the pill. If you’re feeling old-school, feel free to print it out, highlight what you like about each option and bring it in with you to discuss with your GP
- Jump onto the Next Practice app to find leaflets on all of your options
- Visit the Family Planning Victoria website for more information on each method: https://www.fpv.org.au/for-you/contraception
- Book an appointment to have a chat about all of your options with your GP and together make the best decision for you at this time
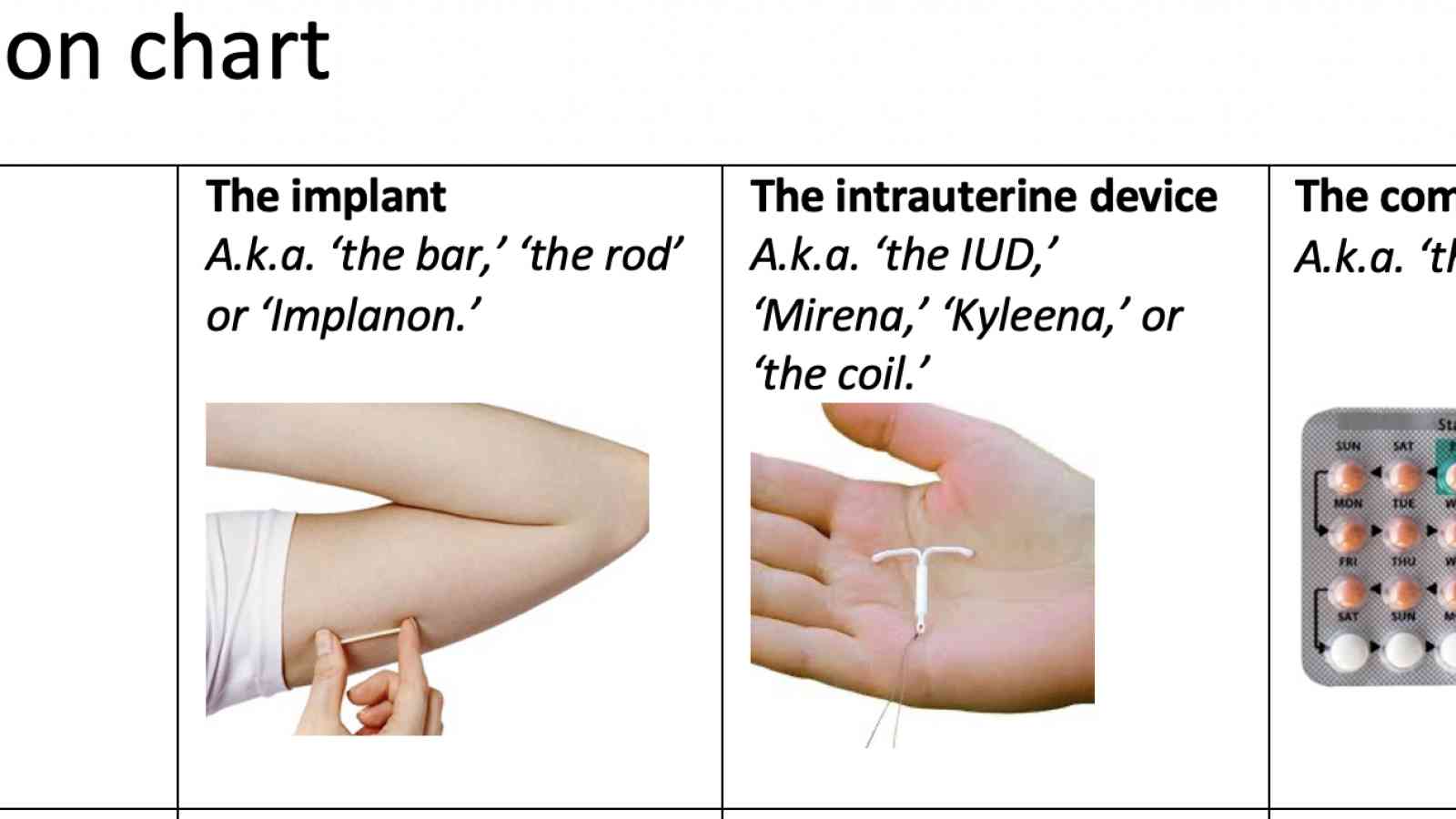
Comparison chart
|
The implant A.k.a. ‘the bar,’ ‘the rod’ or ‘Implanon.’ |
The intrauterine device A.k.a. ‘the IUD,’ ‘Mirena,’ ‘Kyleena,’ or ‘the coil.’ |
The combined pill A.k.a. ‘the pill’ |
|
|
In a year – what are my chances of getting pregnant? |
Less than 1 in 100 |
Less than 1 in 100 |
7 in 100 |
|
How well does it prevent pregnancy? |
99.95% |
99.9% for hormonal 99.5% for copper |
93% (typical use) |
|
What is in it? |
Progesterone |
Progesterone, or Copper |
An oestrogen and a progesterone together |
|
How do I use it? |
A small, rubbery plastic implant is inserted by the doctor under the skin of the arm. The doctor uses a small local anaesthetic injection to numb the area first. It can stay there for up to 3 years. |
A thin plastic device is inserted through the vagina and cervix into the uterus by the doctor. The doctor uses local anaesthetic spray for the procedure to reduce discomfort. The device has soft strings that rest in the vagina for when you want it removed. It can stay there for up to 5 years. |
Swallow one tablet every day, at the same time every day |
|
How often do I have to remember it? |
Every 3 years |
Every 5 years |
Every day |
|
How do I stop it? |
To remove, the doctor provides a numbing injection to the skin, makes a very small cut to the skin, pulls the device out, and brings together with a dressing (no stitches). |
To remove, the doctor does a physical examination to find the IUD strings, and gives them a very gentle, quick pull to remove the device. |
Easy... stop swallowing the pills |
|
How long after stopping it does my normal fertility return? |
Straight away |
Straight away |
Straight away |
|
What costs* are involved? *Prices based on having Medicare |
$40 at the pharmacy + 3 appointments per device lifespan (please ask the desk for current insertion and other appointment costs) |
$40 at the pharmacy + 4 appointments per device lifespan (please ask the front desk for current insertion and other appointment costs) |
$10-$80 (varies) at the pharmacy every 3-4 months, plus yearly doctor appointments |
|
What are the possible side effects and risks? |
Changes in bleeding pattern (see above). Small numbers of women report headaches, skin changes, sore breasts or mood changes which often settle with time. Risks are rare but include the device moving position and damage to the tissues during insertion or removal. |
Changes in bleeding pattern (see above). Small numbers of women report headaches, skin changes, sore breasts or mood changes which often settle with time. Risks are rare but include the device falling out, perforation of the uterus, and pelvic infection. |
Possible side effects include nausea, bloating, skin changes, headaches, breast tenderness, mood changes, changes in libido, chloasma, rash, alopecia, increased blood pressure and thrush. Risks are rare but include DVTs, heart attack and stroke, slightly increased risk of breast cancer and cervical cancer, and liver cancer. |
|
Does it cause weight gain? |
No |
No |
No |
|
Will I get my period while using it? |
Possibly, but it is likely to be lighter. It might be more often or irregular. Around 20% of people using the implant will have no bleeding at all (this is not harmful to the body). Around 20% of people have frequent or prolonged bleeding which may get better with time. If it doesn’t, we can remove it and try another option. |
Hormonal: Probably not. Bleeding and spotting is common initially. By 6 months around 95% of users will have a light regular period or no bleeding at all (this is not harmful to the body). Copper: Yes, and for most users their periods are about 50% heavier. It is therefore not a good option if you already have heavy or painful periods. |
Yes, up to 7 days each month when taking the ‘sugar’ (inactive) pills |
|
So, why would I choose it? |
I want the most effective option (99.95%) I don’t want to have to remember to take a pill every day It might make my periods lighter and less painful I prefer the idea of an implant in the arm because it is minimally invasive |
I want a very effective option (99.90%) I don’t want to have to remember to take a pill every day I am likely to have no periods or far lighter and less painful periods I prefer the idea of a uterine implant because the hormone only works locally on the uterus |
I want an effective option (93%) I don’t want a procedure I want to be able to control when I get my period I want to be able to stop and start my method without the help of my doctor |
Written by Dr Alyssa Kelly


